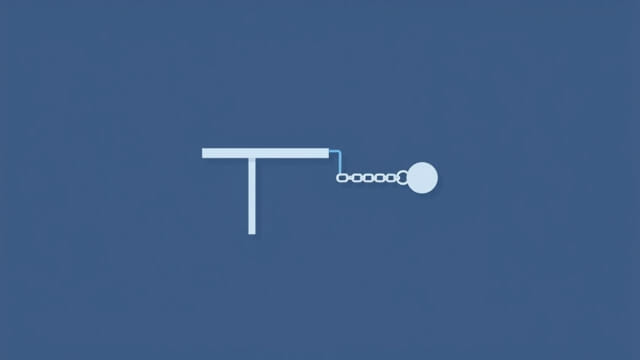
In medical terminology, a flail joint refers to a severely unstable joint that has lost its normal support due to damage to both the bones and the surrounding soft tissues, such as ligaments and muscles. This condition can occur after significant trauma or surgical complications, and it results in abnormal and excessive movement of the joint. A flail joint does not function properly because the structures that usually hold it in place are either absent or too damaged to do their job. As a result, the joint becomes weak, wobbly, and uncontrollable, often leading to serious impairment in movement and stability.
Definition and Characteristics of a Flail Joint
What Makes a Joint Flail
A joint is considered ‘flail’ when it has lost its ability to maintain alignment and control of movement due to the disruption of its stabilizing components. This includes:
- Loss of bone integrity due to fractures or resection
- Severe ligamentous damage or complete rupture
- Muscle paralysis or detachment affecting control
- Loss of mechanical articulation in the joint capsule
These conditions combine to create a joint that lacks resistance to movement in multiple directions. The term is often used to describe joints in the upper or lower limbs, particularly after extreme injury or failed joint replacement surgeries.
Common Locations
Flail joints are most commonly observed in the:
- Shoulder – following a brachial plexus injury or shoulder dislocation
- Elbow – due to extensive trauma or surgical removal of bone segments
- Wrist – often after nerve damage or fracture-related complications
- Hip – particularly in cases of failed hip arthroplasty or dislocation
Causes and Risk Factors
Traumatic Injury
The most frequent cause of a flail joint is high-impact trauma, such as that resulting from motor vehicle accidents, industrial injuries, or falls from significant heights. These types of injuries can lead to complex fractures, dislocations, and soft tissue damage. In cases where bones cannot be repaired or when tissues are beyond reconstruction, a flail joint may develop.
Neurological Damage
Nerve injuries can cause paralysis of the muscles around a joint. Without muscular support, the joint cannot be controlled and loses stability. For instance, damage to the radial nerve in the arm can lead to a flail elbow or wrist.
Post-Surgical Complications
In some cases, flail joints occur after surgical procedures. These include:
- Failed joint replacements (e.g., hip or shoulder prosthesis dislocation)
- Bone resections due to tumors or infections
- Unsuccessful ligament or tendon repair surgeries
Infection, poor surgical planning, or complications during healing can all contribute to the development of a flail joint postoperatively.
Clinical Signs and Symptoms
Visible Instability
One of the most obvious signs of a flail joint is abnormal motion. The joint may appear to dangle or wobble uncontrollably, with movements that are not under voluntary control. Patients often describe the sensation as if the limb is hanging loose.
Loss of Function
Due to the inability to stabilize the joint, patients typically experience a significant loss of function. They may not be able to lift, carry, walk, or perform daily activities depending on the joint involved. Weakness and lack of control make tasks like writing, dressing, or even standing up difficult.
Pain and Discomfort
While some flail joints may be painless if nerves are damaged, others can be accompanied by chronic pain due to instability, muscle fatigue, and secondary inflammation. Overuse of surrounding structures can also lead to compensatory pain.
Diagnosis of a Flail Joint
Physical Examination
Doctors assess joint motion, stability, and alignment through clinical tests. They evaluate muscle tone, reflexes, and sensory response to identify underlying neurological causes.
Imaging Tests
To confirm the presence of a flail joint, medical imaging is essential. These may include:
- X-rays to identify bone loss or dislocations
- MRI scans to view soft tissue injuries
- CT scans for detailed bone structure analysis
- Electromyography (EMG) to assess nerve and muscle function
Combining clinical findings with imaging helps determine the extent of damage and plan for treatment.
Treatment and Management Options
Non-Surgical Approaches
In cases where surgery is not viable or is delayed, conservative management may include:
- Bracing or splinting to stabilize the joint
- Physical therapy to strengthen surrounding muscles
- Assistive devices for mobility (e.g., walkers, canes)
- Pain management through medication or therapy
These methods can improve quality of life and function, but they often provide only limited control of the flail joint.
Surgical Reconstruction
Depending on the location and severity of the flail joint, surgical options may include:
- Joint fusion (arthrodesis) to eliminate movement and stabilize the limb
- Prosthetic joint replacement
- Tendon transfers to restore muscle control
- Bone grafting or reconstruction using implants
Surgical interventions aim to restore function, reduce pain, and improve structural stability. However, outcomes vary depending on the patient’s health, age, and extent of damage.
Prognosis and Quality of Life
Long-Term Outcomes
With proper treatment, some patients regain partial or significant use of the affected joint. Others may need lifelong support from braces or wheelchairs. Early intervention typically leads to better outcomes, especially when nerve damage is minimal and soft tissue structures can be repaired or replaced.
Rehabilitation and Support
Post-treatment rehabilitation is essential. Physical therapy, occupational therapy, and adaptive training help patients relearn how to use their limbs and regain independence. Psychological support is also important, as living with a flail joint can be emotionally challenging.
Prevention and Risk Reduction
Preventing Joint Damage
While not all causes of flail joints are preventable, steps can be taken to reduce risks:
- Use protective gear during high-risk activities
- Seek immediate care for joint injuries
- Follow rehabilitation protocols after surgery or injury
- Manage underlying health conditions that weaken bones and joints
Monitoring Surgical Outcomes
Patients who undergo joint surgeries should be closely monitored for signs of failure or instability. Early detection of complications can allow timely interventions to prevent the joint from becoming flail.
A flail joint is a serious medical condition that results in extreme joint instability and loss of function. It can arise from trauma, surgery, or nerve damage, and affects multiple joints throughout the body. Diagnosis involves both clinical evaluation and advanced imaging. While treatment options vary, from supportive bracing to complex surgery, early recognition and intervention are critical to improving outcomes. Understanding what a flail joint is helps patients, caregivers, and medical professionals manage the condition effectively and work toward recovery or long-term adaptation.