When the heart is unable to fill properly due to pressure from fluid accumulation in the pericardial sac, a serious condition known as cardiac tamponade can occur. This medical emergency affects the heart’s ability to pump blood effectively and leads to several recognizable symptoms. Among these, jugular vein distention, or JVD, is one of the key physical signs that can help doctors quickly identify the presence of cardiac tamponade. Understanding the relationship between cardiac tamponade and jugular vein distention is crucial for both medical professionals and anyone interested in heart health.
Understanding Cardiac Tamponade
Cardiac tamponade occurs when fluid, blood, or other substances accumulate in the pericardial cavity the space between the heart and the pericardium, the thin sac surrounding it. Normally, this space contains a small amount of lubricating fluid that allows the heart to move smoothly as it beats. However, when excess fluid builds up, it creates pressure that compresses the heart, especially the right atrium and right ventricle, which are responsible for receiving blood returning to the heart.
This compression prevents the heart from expanding fully during diastole (the filling phase), leading to a drop in cardiac output. As a result, less blood is pumped to the rest of the body, and venous blood returning to the heart begins to back up, causing symptoms like low blood pressure, shortness of breath, and distention of the jugular veins.
Causes of Cardiac Tamponade
Cardiac tamponade can arise from several underlying conditions. Common causes include
- TraumaPenetrating or blunt injury to the chest can cause bleeding into the pericardial sac.
- PericarditisInflammation of the pericardium, often due to infection or autoimmune diseases, can lead to fluid accumulation.
- Post-surgical complicationsAfter heart or thoracic surgery, bleeding into the pericardial space can occur.
- MalignancyCancer that spreads to the pericardium may cause fluid buildup.
- Uremia or kidney failureToxins can cause inflammation and effusion around the heart.
- Myocardial ruptureFollowing a heart attack, a tear in the heart wall can lead to internal bleeding into the pericardium.
In each case, the key problem is the same fluid in the pericardial cavity restricts the heart’s normal movement, leading to impaired circulation and increased venous pressure.
Jugular Vein Distention A Visible Sign of Pressure
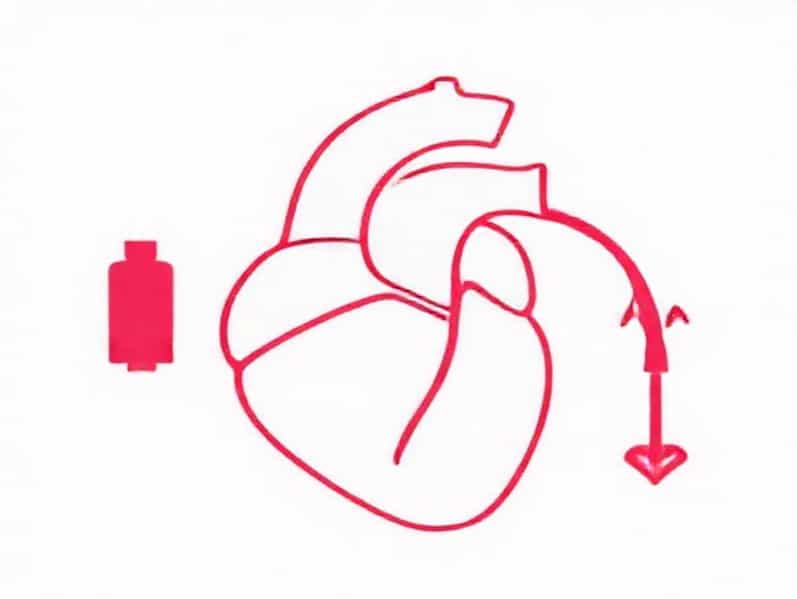
Jugular vein distention, or JVD, refers to the visible bulging of the jugular veins in the neck. These veins carry blood from the head back to the heart, and under normal conditions, they are not prominently visible when a person is sitting or standing. However, when pressure builds up in the venous system due to impaired blood return to the heart as happens in cardiac tamponade the jugular veins become visibly engorged.
JVD is a classic and important physical finding in cardiac tamponade because it indicates increased central venous pressure (CVP). In simple terms, the blood has nowhere to go it’s being blocked from entering the heart efficiently, causing it to pool in the venous system. This distention is often most noticeable when the patient is at a 45-degree angle during examination.
How JVD Develops in Cardiac Tamponade
In cardiac tamponade, the external pressure from accumulated fluid limits the heart’s ability to fill. This leads to elevated pressure in the right atrium and systemic veins. The jugular veins, being directly connected to this system, reflect that increase in pressure. As the condition worsens, the veins may remain distended even during inspiration a finding that helps differentiate cardiac tamponade from other conditions.
In normal breathing, the jugular veins typically collapse slightly during inspiration as the chest expands and draws blood into the heart. But in tamponade, because the heart is unable to fill properly, this normal variation is lost. This absence of jugular venous collapse is known as Kussmaul’s sign, though it is more commonly associated with constrictive pericarditis than with tamponade.
Beck’s Triad Recognizing Cardiac Tamponade Clinically
Cardiac tamponade is often diagnosed based on the presence of a combination of physical signs known as Beck’s triad. These three findings are considered classic indicators of the condition
- Jugular vein distentionElevated venous pressure due to restricted cardiac filling.
- HypotensionLow blood pressure resulting from decreased cardiac output.
- Muffled heart soundsThe heart sounds are faint because the accumulating fluid dampens the vibrations.
The presence of Beck’s triad, particularly in a patient with chest trauma or known pericardial disease, should immediately raise suspicion of cardiac tamponade. However, not all patients show all three signs at once, especially in the early stages, which makes additional diagnostic tools important.
Diagnostic Methods
While jugular vein distention and other physical findings provide important clues, cardiac tamponade is confirmed through diagnostic imaging and monitoring techniques.
1. Echocardiography
An echocardiogram is the most useful test for diagnosing cardiac tamponade. It shows the presence of pericardial fluid and can reveal compression of the heart chambers, particularly the right atrium and right ventricle, during diastole.
2. Electrocardiogram (ECG)
In tamponade, ECG may show low voltage QRS complexes or electrical alternans, a pattern in which the QRS amplitude alternates with each beat, caused by the swinging motion of the heart within the fluid-filled pericardium.
3. Chest X-ray and CT scan
These imaging tests may show an enlarged cardiac silhouette if the effusion is large. However, they are less specific than echocardiography for diagnosis.
4. Hemodynamic Monitoring
Invasive monitoring of central venous pressure or right atrial pressure can confirm elevated filling pressures consistent with tamponade physiology.
Treatment of Cardiac Tamponade
Because cardiac tamponade is a life-threatening condition, treatment must be immediate. The goal is to relieve the pressure on the heart by removing the accumulated fluid from the pericardial cavity.
1. Pericardiocentesis
This is the most common emergency procedure for cardiac tamponade. A needle is inserted into the pericardial space to aspirate the fluid, immediately reducing the pressure on the heart. This can stabilize the patient’s blood pressure and improve venous return, often leading to a rapid decrease in jugular vein distention.
2. Surgical Drainage
In cases where pericardiocentesis is not sufficient, or the effusion is recurrent, surgical creation of a pericardial window allows continuous drainage of fluid.
3. Treating the Underlying Cause
Once the immediate pressure is relieved, the underlying condition that caused the effusion such as infection, trauma, or malignancy must be identified and managed to prevent recurrence.
Differential Diagnosis When JVD Is Not Due to Tamponade
While jugular vein distention is a hallmark sign of cardiac tamponade, it can also appear in other cardiovascular conditions. Some of the most common include
- Right heart failureThe right side of the heart cannot pump effectively, leading to venous congestion.
- Constrictive pericarditisThe pericardium becomes thickened and restricts heart movement, mimicking tamponade physiology.
- Tension pneumothoraxAir trapped in the chest cavity compresses the heart and great veins, causing JVD.
- Superior vena cava syndromeObstruction of venous return from the upper body leads to vein distention.
Therefore, JVD must always be interpreted in the context of other symptoms, medical history, and diagnostic tests to accurately determine its cause.
Prevention and Prognosis
Preventing cardiac tamponade largely depends on managing conditions that can lead to pericardial effusion. Regular monitoring for patients with pericarditis, malignancy, or post-surgical complications is essential. Early detection through imaging can prevent the buildup of significant fluid and avoid the need for emergency intervention.
With timely diagnosis and treatment, the prognosis for cardiac tamponade is generally good. However, if left untreated, it can rapidly progress to cardiogenic shock and death. Recognizing signs like jugular vein distention early can be lifesaving, as it often provides the first visible warning that pressure is building within the pericardial sac.
Cardiac tamponade is a critical condition in which pressure from fluid accumulation around the heart prevents it from filling and pumping properly. Jugular vein distention is one of the most important physical signs that point toward this diagnosis, signaling increased venous pressure and impaired cardiac filling. Understanding the relationship between cardiac tamponade and jugular vein distention helps in early recognition, prompt treatment, and ultimately, saving lives. Awareness of this link is essential for anyone working in healthcare and valuable knowledge for anyone interested in how the heart’s delicate balance can be disrupted by pressure from within its own protective sac.